Credentialing is the method of verifying physician’s qualifications to make it sure that they can give healthcare services to the patients. Credentialing is a fundamental of starting a clinic or healthcare facility because most of the health insurance companies including Medicare, Medicaid and commercial payors requires this to be done before getting paid.

The providers credentialing procedure is accomplished by verifying the provider’s documents to ensure that they are correct and up to date. These provider’s documents include their medical license, DEA, and malpractice insurance. Other than this, following necessary data is required to complete credentialing:
- Medical School Information
- Internships History, Residency Information
- Board Certifications
- Provider’s Resume
Credentialing Services Xceed Billing Solutions Offer
The process of getting any physician credentialed with an insurance company includes too many manual steps which includes filling up application forms, answering to the questions asked by insurances and following up with them to complete the credentialing request. You can keep your data up to date with insurance companies by Xceed Billing Solutions provider credentialing services.
Insurance Credentialing Services We Are Expert In
We are always ready to assist healthcare providers for enrollment with all the insurance companies across USA. Some of the most popular insurance companies for which we are expert in enrollment services are mentioned below:
· Medicare Credentialing Services
· Medicaid Credentialing Services
· Humana Contracting and Credentialing
· Blue Cross Blue Shield Credentialing
· Cigna Contracting and Credentialing
· United Healthcare Contracting and Credentialing
· Aetna Contracting and Credentialing
Why Choose Us for Credentialing and Enrollment Services
Due to our years of expertise in credentialing and contracting, we have strong connections with the insurance credentialing and enrollment representatives which helps us to get you enrolled at earliest. We do our best to get you credentialed and enrolled with your desired insurance companies so that you can start getting reimbursements from those insurance companies as soon as possible.
Xceed Billing Solutions credentialing team delivers a comprehensive and knowledgeable service to help you become an in-network provider with the insurance companies that you want to enrolled with. Also, our medical billing and credentialing services experts can give you recommendations by performing analysis of your service area and specialty, if required.
Providers credentialing is a continuous process and should be done again and again every 2 to 4 years. You will be glad to know that now we are offering credentialing services to existing practices as well. Xceed Billing Solutions provide a re-credentialing service and notify providers about expiring credentialing related documents and maintain your CAQH profile.
What Type of Practices We Deal
We offer credentialing services to both small and large practices, including solo physicians as well as large group of doctors for a group and individual provider credentialing with government and commercial insurances.
Medical Provider Credentialing Process
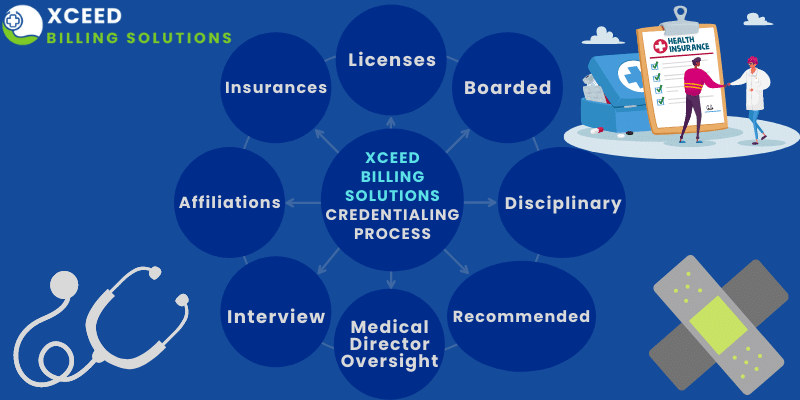
- Medical Credentialing process requires participation of provider, the organization, and the insurance company.
- Normally, the organization provides the healthcare provider with the credentialing applications. Healthcare professional is responsible for completing the given application. Mostly, it is very long with a lot of pages. Also, He or She have to attach all the requested documents. These documents include medical college degrees, board certification, and more. When the given application is complete, the physician submits it to the organization.
- Then organization is responsible for attaching additional documents, which may include, claims history, primary source verification, background screen results, and much more.
- Once the application is completed and appropriate documents are attached, they submit it to the payer.
- The payer analyze the application to decide whether the healthcare provider meets insurance standards or not.
- This complete process is required when the physician first joins a new practice and repeatedly thereafter – usually every 2 to 3 years depending on the payer requirements.
What Information is required for Credentialing?
Required information for credentialing varies from payer to payer but it is relatively consistent across the board and commonly includes the following:
- Malpractice claims history (revocations and revocations)
- Practice license & primary source verification
- NPI Number
- License history
- DEA license
- Work history
- Transcripts and degrees
- References from practitioners/employers
- Board certification
Benefits of Outsourcing Provider Credentialing Services to XBS
Xceed Billing Solutions credentialing services for providers include the following:
- Team of credentialing experts to operate the paper work
- Best credentialing specialist across USA with professional relation with insurance representatives
- Cost and time saving so that you can focus on patients care
- Updates on credentialing status whenever requested by physician
- Let our credentialing experts do the paperwork for you
- Help with the appeals for panel closures
- Major healthcare provider enrollment; Medicaid and Medicare enrollments for individuals and group
- Payments from third-party payers receives much faster
Xceed Billing Solutions Can Help in Credentialing Services
Credentialing can become months of back and forth phone calls and documentation. It is highly time-consuming. Rather than hiring a company that only provides credentialing services, choose Xceed Billing Solutions because we are one-stop shop for all your revenue cycle needs.
